Ask a Physician with Dr. Nicolozakes
Hospice of the Western Reserve recognizes the complexity of making healthcare decisions, particularly in difficult times. Dr. Alexandros Nicolozakes, Associate Medical Director at HWR, has responded to some of the most common questions regarding hospice care.
Will the patient or their loved ones, be a part of the decisions that are made?
Absolutely, not only are patients and their loved ones part of the decisions that are made, but the hospice philosophy also specifically focuses on patient-directed goals, which include family and
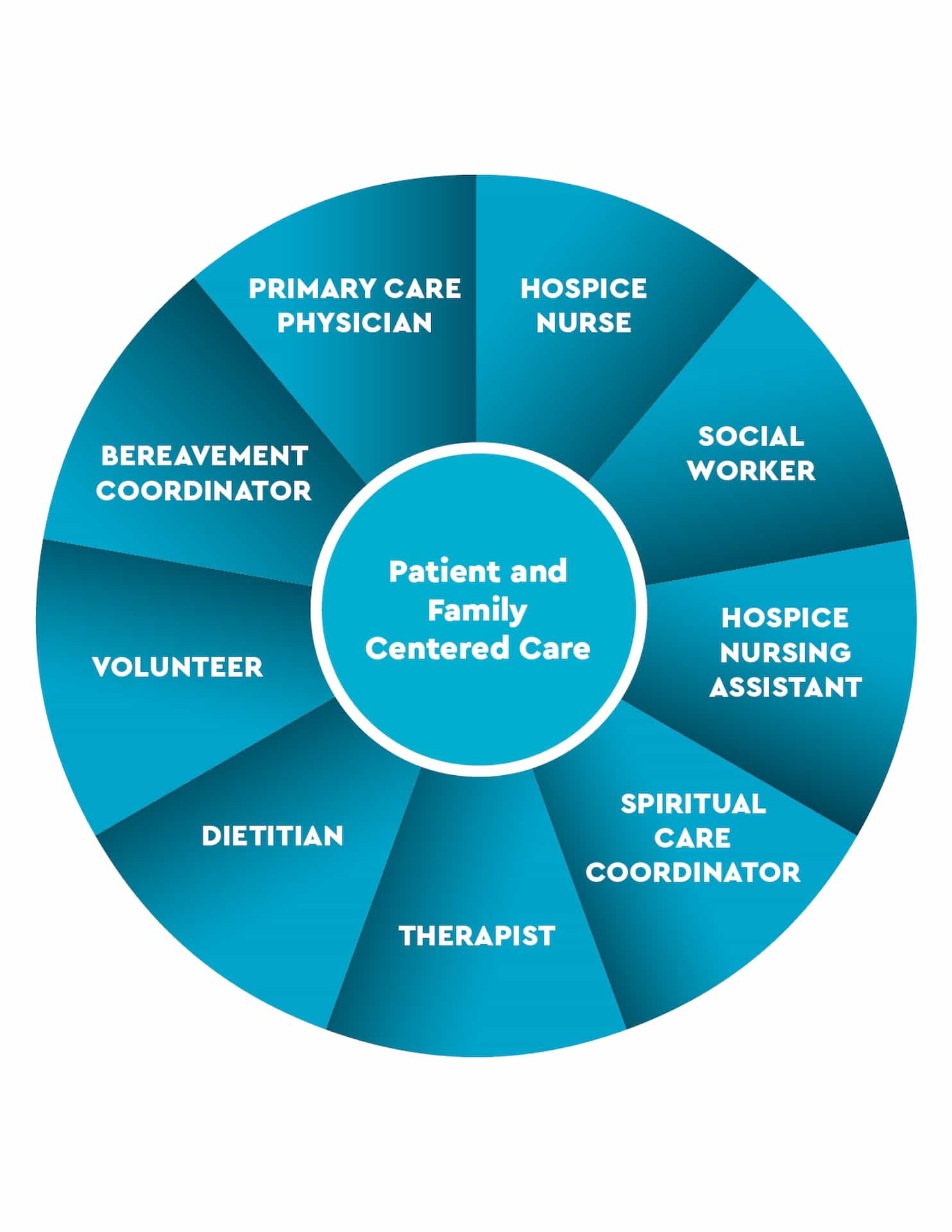
loved ones. This was one of the fundamental concepts of the modern hospice movement developed by Dr. Dame Cicely Saunders. The patient and family are surrounded by a team comprising a physician, nurses, hospice aids, social workers, chaplains, bereavement counselors, and even volunteers.
Can a patient still see their doctor if they want to?
Certainly! The patient retains the freedom to choose. If they prefer to maintain their relationship with their own physician or nurse practitioner, they can do so, with the Medicare benefit covering these hospice-related visits. Additionally, our hospice organization provides a dedicated primary care physician or nurse practitioner to guarantee consistent and uninterrupted care for the patient.
If an individual pursues hospice, does all other treatment stop?
No. While hospice care primarily emphasizes symptom management and avoids extensive diagnostic testing, curative treatments, and repeated hospice admissions, disease-focused interventions may still be employed to alleviate symptoms. For instance, if the patient develops an underlying infection like a urinary tract infection or pneumonia, antibiotics may be administered to enhance the patient’s comfort. In cases of congestive heart failure, appropriate medications can be utilized to address the condition, ultimately improving symptoms, and enhancing the patient’s quality of life.
What happens if a patient gets better?
It is not uncommon for patients to grapple with illnesses that, while not inherently terminal, significantly impact their life expectancy due to their severity. Once enrolled in hospice, however, there’s room for recovery and improvement, particularly when a holistic approach is taken to address both the disease and symptom management. The typical criterion for hospice enrollment is a prognosis of less than six months. Despite this, instances arise where patients experience recovery and improvement beyond this initial estimate. In such cases, patients may surpass the six-month prognosis, leading to their transition out of hospice care.
How long can an individual stay on hospice?
Enrollment in hospice requires a prognosis of less than six months, determined through periodic evaluations by the nurse practitioner and physician, with documented decline for qualification. While some patients, admitted with severe conditions, may pass within days, others may experience a gradual decline and remain on hospice for years. On average, hospice stays last about two months, and 90 percent of patients pass away within the initial six months of enrollment.
.png)
Dr. Alexandros Nicolozakes
Associate Medical Director
Hospice of the Western Reserve
